SIDS Prevention: 7 Safe Sleep Rules Every Parent Must Know (AAP Guidelines)
The thought of a healthy baby suddenly stopping breathing during sleep is every parent's deepest fear. Sudden Infant Death Syndrome(SIDS) remains one of the most devastating and mysterious causes of infant loss. In the United States, approximately 3,400 sleep-related infant deaths occur annually according to the CDC, making it the leading cause of death among infants aged 1 to 12 months. The good news? Safe sleep practices can reduce SIDS risk by up to 50%. This guide covers the 7 essential safe sleep principles from the American Academy of Pediatrics (AAP) that every parent needs to know.
What Is SIDS?
Sudden Infant Death Syndrome (SIDS) is the sudden, unexplained death of an apparently healthy infant under 1 year of age, typically occurring during sleep. Even after a thorough investigation including autopsy, examination of the death scene, and review of the clinical history, no definitive cause of death can be identified.
Key facts about SIDS:
- Most common between ages 2 and 4 months
- About 90% of SIDS cases occur before 6 months of age
- Slightly more common in boys than girls
- Somewhat more frequent during colder months
- Since the 'Back to Sleep' campaign launched in 1994, SIDS rates have dropped by more than 50%
SIDS Risk Factors
While the exact cause of SIDS remains unknown, research has identified several factors that increase the risk.
| Risk Factor | Risk Level | Explanation |
|---|---|---|
| Stomach sleeping (prone) | Very High | Airway obstruction + rebreathing of exhaled CO2 |
| Soft mattress or bedding | High | Face can sink in, increasing rebreathing risk |
| Bed sharing (co-sleeping) | High | Risk of overlay and overheating, especially if parent smokes or drinks |
| Secondhand smoke exposure | High | Smoking during pregnancy more than doubles SIDS risk |
| Overheating (overdressing) | Moderate | Immature temperature regulation → deeper sleep → reduced arousal response |
| Premature or low birth weight | Moderate | Immature brain development weakens arousal response |
| Alcohol use during pregnancy | High | Affects fetal brain development |
7 Rules for Safe Sleep (AAP Guidelines)
These 7 principles are based on the AAP's 2022 updated safe sleep recommendations. Following these guidelines can dramatically reduce your baby's risk of SIDS and other sleep-related deaths.
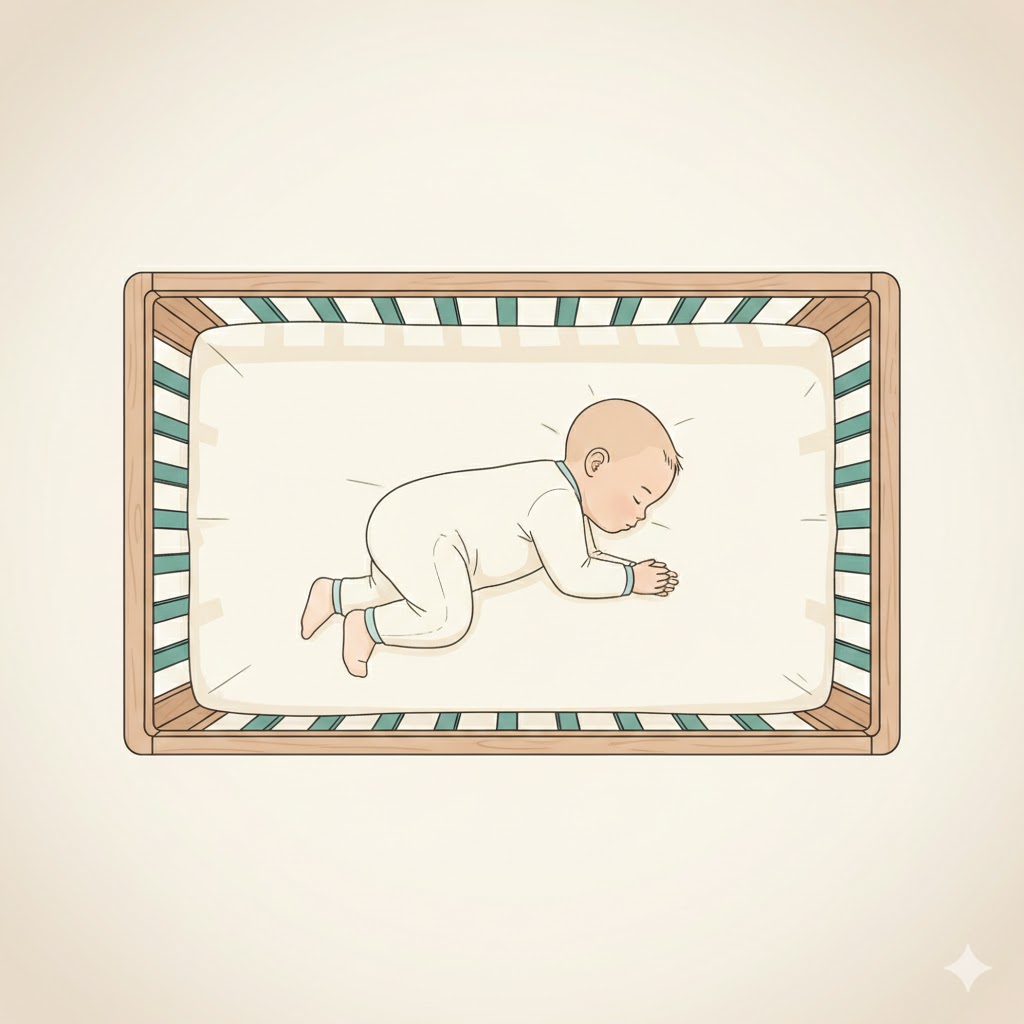
Rule 1: Always Place Baby on Their Back
For every sleep, including naps, always place your baby on their back. This is the single most important thing you can do to reduce SIDS risk.
- Stomach sleeping increases the chance of rebreathing exhaled carbon dioxide (CO2), leading to oxygen deprivation
- Side sleeping is also unstable and can result in rolling to the stomach
- Once baby can roll both ways on their own: It's safe to let them stay in the position they choose. However, always start by placing them on their back
Rule 2: Use a Firm, Flat Mattress
Your baby should always sleep on a firm, flat mattress designed specifically for infants that meets CPSC (Consumer Product Safety Commission) safety standards.
- Why firm? Soft surfaces allow the face to sink in, creating a pocket of CO2 that the baby rebreathes
- Never use inclined sleepers — the FDA has warned against these products due to infant deaths
- Check for gaps: If more than two fingers fit between the mattress and crib frame, it's a hazard
- Never let baby sleep on adult beds, couches, or armchairs
Rule 3: Keep the Crib Bare
The only thing in your baby's crib should be a tightly fitted sheet. Everything else must go.
- Remove: blankets, pillows, bumpers, stuffed animals, cushions, and loose bedding
- Alternative for warmth: Use a sleep sack (wearable blanket) instead of loose blankets
Rule 4: Room Share, Not Bed Share
Share a room with your baby, but not a bed. The AAP recommends room sharing for at least 6 months, ideally up to 1 year.
- Why room sharing helps: Your nearby presence promotes baby's arousal responses, reducing SIDS risk by approximately 50%
- Makes nighttime feeding and monitoring easier
- Important: Bed sharing (co-sleeping) is different — it increases risk
- Never fall asleep with your baby on a couch or armchair — this is one of the most dangerous sleep situations
Rule 5: Prevent Overheating
When babies overheat, they sleep more deeply, making it harder for them to wake up in dangerous situations.
- Keep room temperature at 20–22°C (68–72°F)
- Dress baby in no more than one extra layer compared to what you'd wear
- Don't put a hat on baby for indoor sleep — it interferes with heat dissipation through the head
- Use a sleep sack instead of blankets
Rule 6: Offer a Pacifier
Offering a pacifier at nap time and bedtime has been shown to reduce SIDS risk in multiple studies.
- If breastfeeding, wait until breastfeeding is well established (around 3–4 weeks) before introducing a pacifier
- Don't reinsert if it falls out after baby falls asleep
- Don't force it if baby refuses
- Why it helps: The pacifier helps keep the airway open and promotes the arousal response
Rule 7: Breastfeed If Possible
Breastfeeding is associated with a reduced risk of SIDS.
- Breast milk boosts the immune system and promotes lighter sleep, making it easier for baby to wake up in risky situations
- Partial breastfeeding still helps — you don't need to exclusively breastfeed to see benefits
- If breastfeeding isn't possible, don't worry — the other 6 principles alone can significantly reduce SIDS risk
Common Myths vs Facts
There's a lot of misinformation about SIDS. Here are the facts.
| Myth | Fact |
|---|---|
| "Babies sleeping on their back will choke on vomit" | The airway sits above the esophagus, so regurgitated fluid drains away from the airway by gravity. Back sleeping is actually safer. |
| "Co-sleeping is safer for bonding" | Bed sharing increases SIDS risk. Room sharing with separate sleep surfaces is the safest approach. |
| "SIDS is completely unpredictable and unpreventable" | While the exact cause remains unknown, safe sleep environments have reduced SIDS rates by over 50% since the 'Back to Sleep' campaign. |
| "You must turn baby back over if they roll" | If your baby can roll both ways independently, let them find their own position. Always start on the back, but don't worry about repositioning a baby who can roll. |
| "A fan prevents SIDS" | While one study suggested reduced risk, the AAP does not include fan use in its official recommendations. Good ventilation helps, but a fan alone is not a prevention strategy. |
Safe Sleep Checklist
Review this checklist every night before putting your baby to sleep.
- ✅ Baby is always placed on their back to sleep
- ✅ A firm, flat mattress is used
- ✅ No blankets, pillows, or stuffed animals in the crib
- ✅ Baby sleeps in the same room but not the same bed as parents
- ✅ Room temperature is maintained at 20–22°C (68–72°F)
- ✅ A pacifier is offered at sleep time
- ✅ Baby is not overdressed
- ✅ No sleep positioners or inclined products are used
- ✅ No one smokes near the baby
- ✅ A sleep sack is used instead of loose blankets
Winter Safety Tips
During winter, it's tempting to pile on blankets to keep your baby warm — but this can actually increase SIDS risk through overheating.
Winter safe sleep practices:
- Use a sleep sack (wearable blanket) instead of thick blankets
- Never place baby on a heated mattress pad or electric blanket — risk of overheating and burns
- Don't put a hat on baby for indoor sleep — it traps heat
- Keep heaters at a safe distance from the crib
- Use a humidifier to maintain proper humidity (40–60%)
Related Articles
Track Sleep with BebeSnap
Keep your baby's sleep safe and well-documented with the BebeSnap app.
- Sleep Pattern Tracking: Record sleep times and wake-ups to identify patterns
- AI Health Consultation: Ask our AI chatbot about sleep safety and any baby health concerns
- All-in-One Parenting: Track sleep, feeding, diapers, and growth milestones in one app
👉 BebeSnap Sleep Recording Guide
Frequently Asked Questions
Q: If my baby rolls onto their stomach, should I turn them back?
A: If your baby can roll both ways independently, it's safe to let them sleep in their preferred position. However, always place them on their back initially. Once rolling begins, stop using swaddles immediately.
Q: Is swaddling safe?
A: Swaddling is safe before your baby shows signs of rolling, as long as it's done correctly — hips loose, chest snug enough for 2–3 fingers. Stop swaddling immediately when rolling signs appear. A swaddled baby on their stomach is extremely dangerous.
Q: Are crib bumpers safe?
A: The AAP recommends against all crib bumpers. In the U.S., federal law has banned the sale of crib bumpers since 2022. Even mesh bumpers are not recommended, as their safety has not been proven.
Q: What's the difference between SIDS and suffocation?
A: SIDS is diagnosed when no cause of death is found even after autopsy and investigation. Suffocation occurs when the airway is physically blocked. Safe sleep environments help prevent both.
Q: Do baby breathing monitors prevent SIDS?
A: The AAP states there is insufficient evidence that breathing monitors prevent SIDS. Don't rely on monitors — focus on creating a safe sleep environment instead.
References
Manage Easier with BebeSnap
AI stool analysis, feeding & sleep tracking, health reports—all in one app.
You Might Also Like

Baby Eczema vs Infant Heat Rash | Symptoms, Skincare & When to See a Doctor
Is your 2-3 month old's face turning red? Heat rash resolves before age 1, but atopic dermatitis persists 2+ months. Maintain 50-60% humidity and moisturize 2-3 times daily.

Baby Choking First Aid: Complete Guide to Infant Back Blows, CPR & Prevention
Baby choking on food and can't breathe? For infants under 1, give 5 back blows + 5 chest thrusts — NOT the Heimlich. Step-by-step first aid guide.

Baby Cold Symptoms & Treatment: Complete Guide from Newborn to 12 Months
Is your baby showing cold symptoms? Learn age-specific symptoms, home care tips, and warning signs that require medical attention.